444
Views & Citations10
Likes & Shares
CASE REPORT
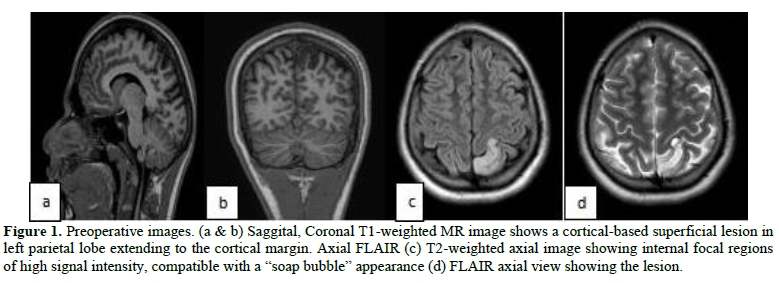
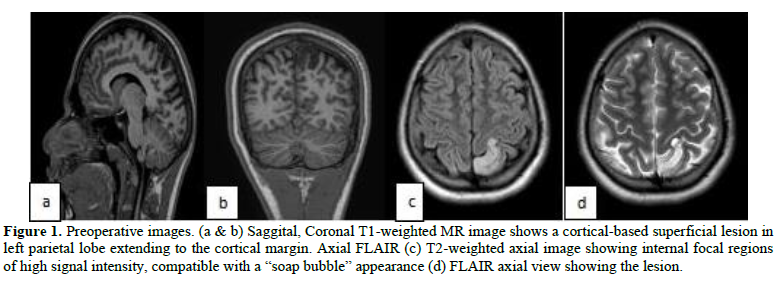
A 16year adolescent male presented with sensory seizures for the last 7 years. Seizure semiology starts with abnormal sensation in his right lower limb lasting for 2 -3 minutes, followed by feeling of numbness, tingling and heaviness over the right lower limb with loss of consciousness for 10 minutes. His first seizure episode started at the age of 9 years for which he was started on single anti-epileptic drug (AED). After 2 years he discontinued AED and was seizure free for 2 years. Again, he developed an episode of sensory seizure, for which he was again started on AED. No imaging was done at that time. Later the frequency of seizure episodes increased 4 to 5 episodes per week and AED was increased to four gradually. Then he was referred to our hospital, MRI brain with seizure protocol was done showing a cortical mass with hypointense in T1-weighted images (T1WI) and hyperintense in T2-weighted images (T2WI) and FLAIR sequences without surrounding perilesional edema or signs of mass effect. No contrast enhancement and appear as an enlarged heterogeneous gyrus, with delicate septa-like structures that are visible within the lesion, producing a soap-bubble appearance at the cortical margins reported as DNET with FCD (Figure 1). Electroencephalogram (EEG) was done, epileptogenic activity correlating with the lesion. All necessary Preoperative work up was done and planned for awake craniotomy with neuro navigation guidance and safe maximal excision of the lesion.
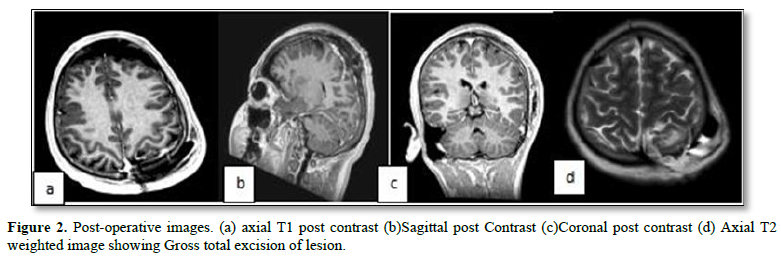
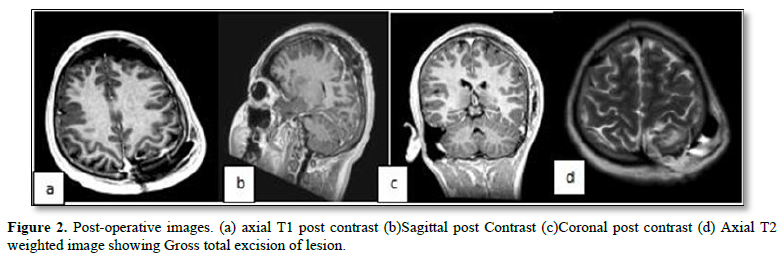
Under scalp block and LA patient in supine position, with the help of neuro navigation, skin incision marked, mini craniotomy done. Pre-operative EEG showed an epileptic focus. Lesion identified with help of neuro navigation. Intra operatively patient was advised to move his right upper and lower limb continuously. At a point where patient developed a mild right lower limb weakness the resection was stopped. Near total excision of lesion was done (Figure 2). Postoperative EEG showed no epileptic discharge.
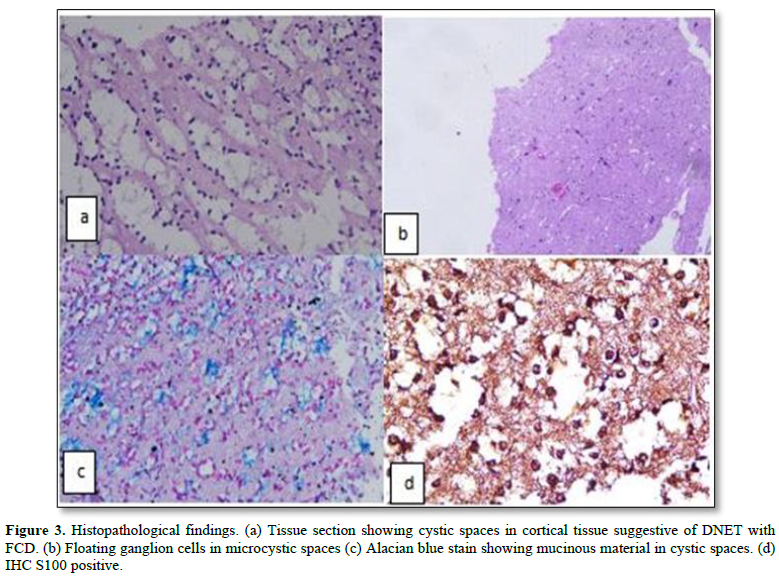
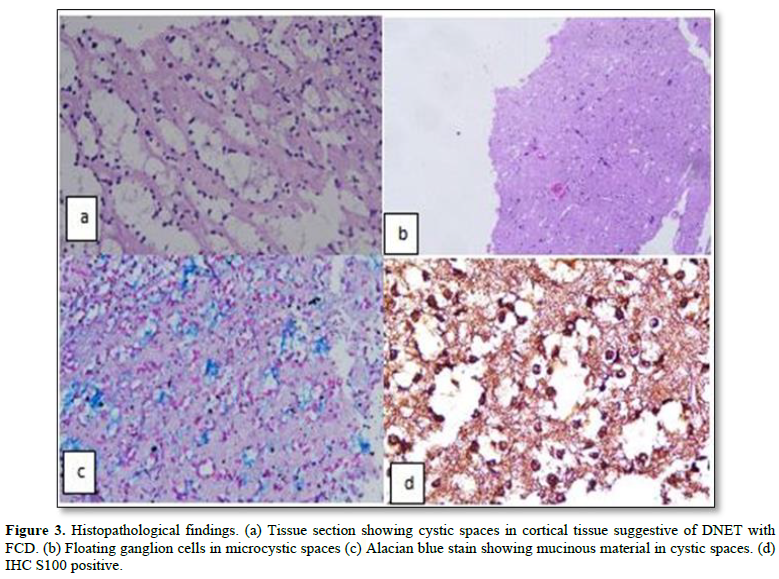
Histopathology reported as DNET with FCD. IHC markers: S100 - Positive on tumor cells. Synaptophysin - Positive on few floating neurons. GFAP-Negative (Figure 3).
DISCUSSION
Dysembryo plastic neuroepithelial tumors (DNETs) are an uncommon, benign type of tumor of neuroepithelial origin that arises from the cortical gray matter. Daumas-Duport coined the phrase "DNET". The temporal lobe (62%) and frontal lobe (31%) are the two most frequent sites [1]. DNETs can develop in the caudate nucleus, cerebellum, or pons, albeit the majority of them are only found in the cortical gray matter [2]. Intractable seizures are the typical presentation in terms of clinical symptoms. Cortical dysplasias are commonly seen with DNETs, occurring in nearly 50 % of cases [3]. Focal cortical dysplasia (FCD) is a diverse group of cortical lesions.
In the review of literature, Lee [4] in his series of 23 patients only one had lesion in parietal lobe [4]. Takahashi [9] in his series of 24 cases no cases were reported in parietal lobe had sensory seizures. Prayson [5] in the series of 52 patients with cortical dysplasia only 4 had in parietal lobe [5].
The majority of cortical dysplasias are caused by neuronal migration abnormalities that occur before the twenty-fourth week of pregnancy [6].
DNET's are typically cortical lesions that lack significant mass effect or peri-tumoral edema. DNET typically shows up as intracortical masses on MR imaging that are hypointense on T1-weighted images and hyperintense on T2-weighted images without any perilesional edema or mass effect indicators in the surrounding area. Differential diagnosis are oligodendrogliomas, gangliogliomas, and astrocytomas.
DNETs can vary greatly in terms of size and shape, but they typically have a friable consistency and are mucinous, multinodular, or muticystic lesions [7]. Microscopically, DNETs are composed of multiple nodules containing both neuronal and glial components. They are characterized by an admixture of astrocytes and oligodendroglial elements, in association with “floating neurons” and mucinous degeneration [7]. The multinodular pattern and areas of mucinous degeneration observed on histopathology may contribute to a soap- bubble appearance on neuroimaging. Other common histological features include “specific glioneuronal elements” oriented in a columnar pattern, perpendicular to the cortical surface and focal areas of cortical dysplasia [8].
We could see that this epilepsy surgery-oriented approach could cure patients with DNET, which is essentially a benign tumor. Patients can be free of tumor recurrence with complete tumor resection and seizure without antiepileptic drugs with complete resection of epileptogenically active areas in and around the tumor [9].
Complete removal of the lesion (total resection of the tumor microscopically and macroscopically) may be required to achieve favorable seizure control, but it is not sufficient to achieve cure levels (complete seizure freedom without medication). We believe that DNET, particularly when associated with CD, may have a similar epileptogenic mechanism as intractable epilepsy associated with CD, which we previously reported [10].
Excellent seizure control could be attributed to a combination of thorough preoperative evaluation, radical resection, and meticulous electrophysiological investigation.
CONCLUSION
DNET is commonly associated with Cortical dysplasia and appears to contribute to DNET's epileptogenic activity. For optimal disease treatment, surgical treatment should aim to remove both DNET and FCD. Very few cases of parietal DNET with FCD causing pure intractable sensory seizures were reported in literature so far makes this case rare entity. Awake craniotomy along with neuro navigation helps to achieve safe maximal resection in eloquent areas with minimal or no deficits.
DECLARATION OF PATIENT CONSENT
The authors certify that they obtained all appropriate patient consent forms. In the form the patient has given his images and other clinical information to be reported in journal. The understood that his name and initial will not be published and due to efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
CONFLICT OF INTEREST
The authors declared that there are not conflicts of interests.
- Daumas-Duport C, Pietsch T, Lantos PL (2000) Dysembryo plastic neuro epithelial tumor. In: Kleihues P, Cavenee WK, Pathology and genetics of tumors of the nervous system. Lyon, France: IARC pp: 103-106.
- Cervera-Pierot P, Varlet P, Chodkiewicz JP, Daumas-Duport C (1997) Dysembryoplastic neuroepithelial tumors located in the caudate nucleus area: Report of four Neurosurgery 40(5): 1065-1070.
- Frater JL, Prayson RA, Morris HH, Bingaman WE (2000) Surgical pathological findings of extratemporal-based intractable epilepsy: Astudy of 133 consecutive resections. Arch Pathol Lab Med 124: 545-549.
- Lee J, Lee BL, Joo EY, Seo DW, Hong SB, et al. (2009) Dysembryoplastic neuroepithelial tumors in pediatric patients. Brain Dev 31(9): 671-681.
- Prayson RA, Estes ML (1995) Cortical dysplasia: A histopathologic study of 52 cases of partial lobectomy in patients with Hum Pathol 26(5): 493-500.
- Kaufman WE, Galaburda AM (1989) Cerebrocortical microdysgenesis in neurologically normal subjects: A histopathologic Neurology 39: 238-244.
- Daumas-Duport C, Scheithauer BW, Chodkiewicz JP, Laws ER, Jr, Vedrenne C, et al. (1988) Dysembryoplastic neuroepithelial tumor: A surgically curable tumor of young patients with intractable partial Neurosurgery 23(5): 545-556.
- Koeller KK, Henry JM (2001) Superficial Gliomas: Radiologic-Pathologic Radio Graphics 21(6): 1533-1556.
- Takahashi A, Hong SC, Seo DW, Hong SB, Lee M, et al. (2005) Frequent association of cortical dysplasia in dysembryoplastic neuroepithelial tumor treated by epilepsy Surg Neurol 64(5): 419-427.
- Hong SC, Kang KS, Seo DW, Hong SB, Lee M, et al. (2000) Surgical treatment of intractable epilepsy accompanying cortical J Neurosurg 93: 766-773.
QUICK LINKS
- SUBMIT MANUSCRIPT
- RECOMMEND THE JOURNAL
-
SUBSCRIBE FOR ALERTS
RELATED JOURNALS
- Journal of Cardiology and Diagnostics Research (ISSN:2639-4634)
- International Journal of Clinical Case Studies and Reports (ISSN:2641-5771)
- Dermatology Clinics and Research (ISSN:2380-5609)
- Journal of Cell Signaling & Damage-Associated Molecular Patterns
- Stem Cell Research and Therapeutics (ISSN:2474-4646)
- Journal of Spine Diseases
- Oncology Clinics and Research (ISSN: 2643-055X)